T Cell Immunotherapy Opens New Doors to Surviving Blood Cancers
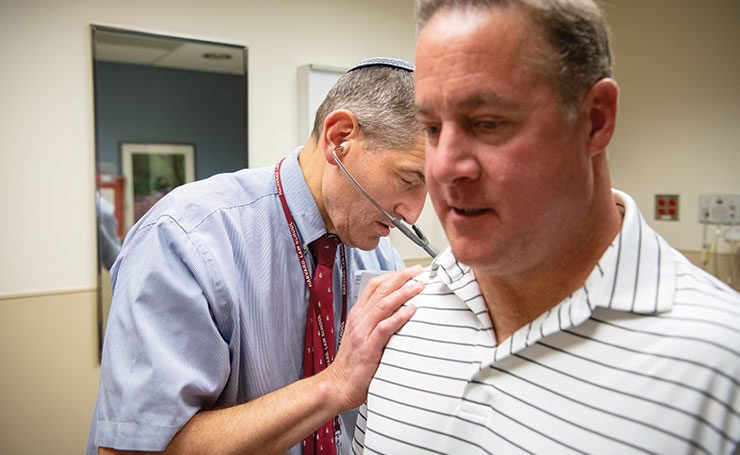
To say that Gary Gardiner Jr. is a fan of the medical team at the University of Maryland, Baltimore (UMB) is more than an understatement. The 49-year-old former Virginia police detective turned real estate executive credits UMB, its School of Medicine (SOM), the Greenebaum Comprehensive Cancer Center, and the University of Maryland Medical Center with saving his life.
And Gardiner is so thankful that he and his wife, Teresa, now travel to medical conferences around the country to relate his story and the benefits of CAR-T therapy, the cancer immunotherapy that UMB oncologists have been at the forefront of developing, testing, and bringing to patients.
Before looking further into what Gardiner calls his “cancer journey” it’s appropriate to revisit the path of the therapy that saved his life. The idea to develop cancer immunotherapies using the patient’s own immune cells that have been modified to fight cancer cells goes back a decade or more.
Today, through persistent development and new technologies, immune therapy has become a reality for patients who have failed other cancer treatments and are left with no other treatment options for the aggressive disease.
“Our research is focused on developing therapies that activate a patient’s immune response to recognize and destroy tumors,” says Kevin Cullen, MD, director of the Greenebaum Cancer Center and a professor of medicine at SOM. “Tumor immunology includes adoptive cell transfer [ACT], which has emerged as a powerful, targeted immunotherapy.”
One such ACT immunotherapy is called “CAR-T,” in which a patient’s immune system T cells — cells critical to generating the body’s natural immune response — are retrieved, “engineered” to target specialized protein receptors on tumor cells, then infused back into the patient. “CAR” refers to “chimeric antigen receptors.”

“The receptors are called ‘chimeric’ because they combine antigen-binding and T cell-activating functions into a single receptor,” explains Cullen, who has led the Greenebaum Cancer Center to national prominence during the past 14 years. “These special receptors allow the T cells to recognize and attach to a specific protein on tumor cells and kill cancer cells. CAR-T therapy is considered a ‘living drug’ because the infused T cells expand and proliferate throughout the patient’s body.”
Aaron Rapoport, MD, SOM’s Gary Jobson Professor in Medical Oncology, working with Carl June, MD, of the University of Pennsylvania’s Abramson Cancer Center, helped pioneer T cell immunotherapy for blood cancers. Rapoport explains the importance of the immune receptor known as CD 19 — a kind of immune cell protein — for CAR-T therapy’s ability to target and attack certain types of cancer cells.
“There are many immune system proteins, but CD 19 is expressed on B-cells in lymphomas, such as non-Hodgkin lymphoma,” explains Rapoport. “We reprogram a patient’s T cells to specifically target CD 19 on cell surfaces.”
While modifying T cells to attack tumor cells is one of the most important aspects of CAR-T therapy, most cancer centers send a patient’s T cells away to an independent lab for modification. However, the Greenebaum Cancer Center now has its own lab, called the “FACT” lab, where the T cells are engineered “in house” to be targeted cancer fighters.
“It’s a very clean space where cells can be manipulated and modified,” says Rapoport, adding that generous financial gifts from Peter Angelos and Neil Kishter helped the lab become a reality.
CAR-T is not for all patients, nor is it for all cancers, says Rapoport.
“It is designed for patients who have B-cell lymphomas and, having failed chemotherapy and radiation, have no other treatment options,” he explains.
To date, CAR-T has been a success. According to Rapoport, the Greenebaum center has used CAR-T therapy to treat more than 50 patients with relapsed and refractory aggressive lymphoma or acute leukemia. More than one year after CAR-T treatment, 85 percent of those patients are still alive and more than 50 percent are in complete remission.
CAR-T as a lifesaver
One of them is the aforementioned Gardiner. In early 2017, after having several illnesses misdiagnosed, he was diagnosed with non-Hodgkin lymphoma. His was a very aggressive cancer and he went through nine cycles of failed chemotherapy and 30 days of radiation.
Fortunately, his local oncologist knew about advances in cancer immune therapy and put him in touch with Rapoport. The Gardiners came to Baltimore and stayed at a hotel not far from the Medical Center while Gary went through the CAR-T steps. They continued to run their real estate business from their hotel suite.
The care team collected his T cells on April 12, 2017, and sent them to California to be re-engineered. The modified T cells were infused back into him on May 7. Following the infusion, he was immediately hospitalized in anticipation of side effects. On May 10, he developed cytokine release syndrome (CRS), a systemic inflammatory response. CRS,the most common type of toxicity caused by CAR-T cell infusion,can lead to widespread organ dysfunction. He was continuously monitored by a medical team that included 15 doctors.
After he was released from the inpatient unit on May 15, the Gardiners stayed in Baltimore, returning to the hospital daily for checkups after his infusion, then checkups three days a week, then two days a week. Finally, on June 12, they returned to Virginia. Gardiner was in full remission. He had no traces of cancer.
“They saved my life,” says Gardiner. “The collaboration between doctors was incredible.”
The future of adoptive cell therapy
According to Rapoport, SOM researchers are developing the next generation of CAR-T therapy adaptable to lymphomas, and perhaps even immunotherapy for solid tumor cancers, such as targeting the antigen present in prostate cancer. Research and testing also is underway to find therapeutic agents that selectively target CD 22, another member of the B-cell antigen family similar to CD 19.
“The field of immune therapy will revolutionize the care of cancer patients,” Cullen says. “In a few years, it will completely change how we treat cancer patients, and that will be vastly different treatment from how we treated patients 30 years ago. The University of Maryland Greenebaum Comprehensive Cancer Center is committed to groundbreaking and lifesaving research efforts, from cancer vaccines to CAR-T cell therapy. It’s a huge team effort.” C